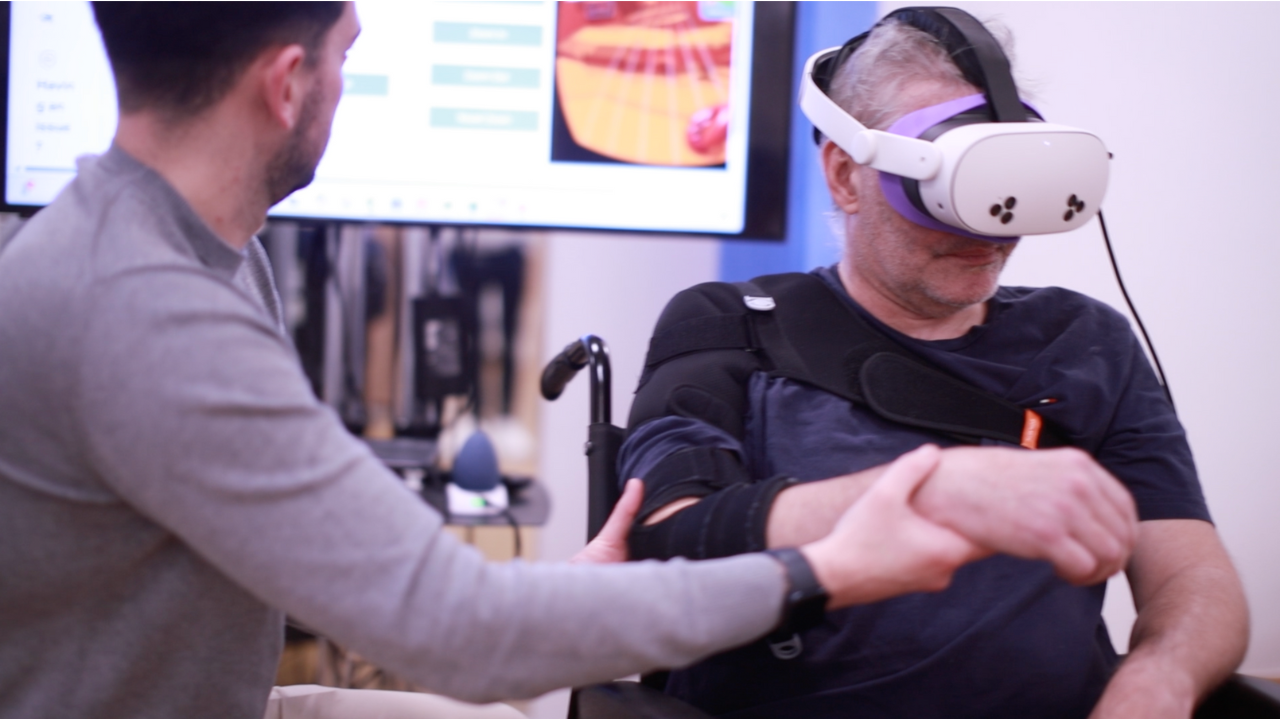
In a quiet lab, the headset slips into place. On the screen, a patient’s hand reaches out, hesitant at first, toward a shimmering object in a virtual garden. Small movements matter here. Each lift, each extension, is logged and gently corrected by unseen algorithms. The patient isn’t playing a game. Instead, they are reclaiming functions that a stroke once tried to take away.
At the heart of this shift is Dr. Eve Gregoriou. A PhD neuroscientist by training, who spent years studying brain stimulation techniques at University College London (UCL), working to understand how to optimize motor recovery for stroke survivors through the use of neurotechnology. Dr. Gregoriou kept running into a deeper problem: therapy wasn’t reaching enough people, and when it did, it wasn’t reaching them often enough.
“I had yet to see systems that were not bulky, clinic-bound, and focused solely on movement quality,” they recall. "There was little done to empower patients outside of therapist-supervised sessions." Around the same time, commercial virtual reality (VR) headsets were quietly evolving, no longer devices for gaming, but portable, affordable platforms with sophisticated tracking capabilities.
From lab concept to home rehab
Dr. Gregoriou saw the opportunity to help those suffering from strokes and founded NeuroVirt in early 2020, a company dedicated to rethinking stroke rehabilitation. Through immersive extended reality (XR) and advanced artificial intelligence (AI), NeuroVirt delivers high-dose therapy at home and in clinics. It offers patients a way to continue rehabilitation beyond traditional walls, maintaining both intensity and quality without needing expensive or intimidating equipment.
Rather than focusing on a single metric to measure movement success, NeuroVirt’s system blends a range of indicators: range of motion, speed, smoothness, layered with context-specific insights like fatigue and compensatory behaviors. “Rehabilitation is inherently multidimensional,” Dr. Gregoriou explains. “Our AI is particularly adept at detecting and classifying compensatory movements, which are often subtle yet clinically significant.”

For clinicians, NeuroVirt provides a clear window into patient progress. Rather than overwhelming therapists with raw data, the system highlights trends over time, adherence to therapy, and significant changes in movement patterns. Safety flags and contextual notes add an extra layer of reassurance, giving therapists a way to monitor without being on call for every session.
Making therapy feel like play
Building NeuroVirt also meant venturing into uncharted territory: gamifying healthcare. Dr. Gregoriou is clear that there’s no playbook for this. Through co-design with patients and clinicians, the NeuroVirt team learned that adapting to physical capabilities wasn’t enough. Sessions needed to respond in real time to changes like fatigue. This led to the development of dynamic adjustment algorithms that tailor difficulty and pacing as the patient moves through exercises, keeping them engaged without overexertion.

As the hardware evolves, NeuroVirt stays ready. The software was designed from the start to be hardware-agnostic, ensuring that a patient using a VR headset today will have no trouble transitioning to lightweight AR glasses in the future. “Our code allows for rapid adaptation,” says Dr. Gregoriou. “It provides a seamless experience without sacrificing quality.”
Expansion hasn’t stopped at the upper body. NeuroVirt’s latest modules target gait and balance, two areas critical to independence after a stroke. Here, subtle foot-placement errors are tracked and addressed through positive feedback and intuitive environmental cues. The goal is to create a feeling of mastery, not a reminder of limitation.
Scaling the vision
Behind the scenes, NeuroVirt balances creativity with the demands of medical regulation. Game environments and narrative layers can evolve quickly, keeping the experience fresh, while core therapeutic modules undergo structured validation. NeuroVirt’s team maintains a careful balance of clinical integrity and patient engagement through this approach.
To build NeuroVirt’s team, Dr. Gregoriou looks for more than technical skills. Candidates are asked to design gamified rehab activities that integrate clinical knowledge and emotional engagement. “The most promising candidates ask critical questions about patient needs, impairment profiles, and therapy goals”.
Backed by $5 million in funding from grants and venture capital, NeuroVirt is scaling steadily. Investors have helped sharpen the company's focus, pushing the team to define the value and return on investment for new features, a discipline that ensures each addition moves the platform closer to real-world impact.
By 2030, Dr. Gregoriou envisions NeuroVirt becoming a first-line therapy option, not an afterthought. Faster recoveries, fewer hospital readmissions, and better quality of life for stroke survivors are more than goals. They are the outcomes NeuroVirt is quietly and steadily working toward. One patient, one movement, one headset at a time.
